Gilbert’s Syndrome and High Bilirubin: Learn Hidden Cause of Gut/Brain Issues
Signs and Symptoms of Gilbert’s Syndrome in Adults
My new ONLINE COURSE for Gilbert’s Syndrome is here! The most complete resource on Gilbert’s Syndrome: Living with Gilbert’s Syndrome – True Health Synergy (simplero.com)
You can also follow my Instagram page Gilberts_Syndrome_Support for all things Gilbert’s, my clinical insights and recommendations.
Common Symptoms that people with Gilbert’s Syndrome experience:
Do you find that your bowel movements are all over the place regardless of whether you eat the same foods?
Do you suffer from constipation or loose stools, especially stools in yellow/mustard colour that float (sorry for the gory details)?
Have you ever had yellowing of skin/eyes -jaundice?
Are you often really fatigued for no reason?
Has your gallbladder been taken out, or have your parents/grandparents had gallbladder issues or had it removed?
Do you feel nauseous after eating fatty foods or generally struggle to digest fats?
Do you struggle to tolerate alcohol, even in small amounts?
Have you been diagnosed with SIBO or IBS?
Do you suffer from depression and/or anxiety?
Do you suffer from estrogen dominance period symptoms: heavy periods, painful periods, shorter or longer cycle length, PMS?
Is your Bilirubin high on blood tests?
People with Gilbert’s Syndrome have a higher predisposition to these issues.
High Bilirubin on blood tests
Gilbert’s Syndrome presents as high Bilirubin on standard Biochemistry blood test results. Chances are you’ve been told constantly high Bilirubin is ‘benign’ and nothing to worry about. This is far from the truth.
Gilbert’s Syndrome is genetic and involves several SNPs (genetic polymorphism- variation) on the UGT1A1 gene/enzyme. This is usually only picked up on a gene analysis like 23andme and is something I test for in-clinic when I see continuously high bilirubin levels on my clients’ blood test results.
Often there are other enzymes in the glucuronidation area (one of the liver’s key phase 2 detox pathways) that are not functioning 100%.

Genetic research shows that over 75% of those with Gilbert’s Syndrome have multiple SNPs that affect the glucuronidation pathway in the liver.
The glucuronidation enzymes are crucial to phase 2 detox in the liver in its job of toxin removal, and in people with UGT polymorphisms, these enzymes function at only 30-50% capacity.
This means that people with Gilbert’s have a much lower ability to clear out toxins from the liver. Also, if they are female, there is often a reduced ability to break down and detoxify hormones such as estrogen. This often leads to numerous hormonal symptoms and can be very pronounced during times of hormonal disruption: puberty, pregnancy, and menopause.
Often people with Gilbert’s are born with jaundice that is resolved in the hospital at birth using light machines. Of course, there are other reasons for high Bilirubin in bloods, such as hepatitis and liver cirrhosis. That’s why confirming with a genetic test is valid.
Often Gilbert’s disease begins to express during puberty (this can be the first time that high Bilirubin is noticed on blood tests), which is a time of hormonal upheaval with a massive influx of hormones needed to be broken down and detoxified by the liver’s glucuronidation pathway.
Most of my patients who test positive for Gilbert’s Syndrome have digestive and psychological symptoms such as depression and anxiety.
Studies have shown that only about 10% of people with Gilbert’s Syndrome are asymptomatic.
The reason I have been researching Gilbert’s Syndrome is that I have the gene and the Syndrome. I have had high bilirubin levels my entire life, undiagnosed until I tested for the gene later in life.
My anecdotal clinical experience shows that many people who have high Pyrroles often also have Gilbert’s Syndrome, and my theory is that this is due to the liver’s poor ability to break down haem. Bilirubin and Pyrroles are both by-products of haem breakdown in the glucuronidation pathway in the liver.
Furthermore, many people with Gilbert’s do not do well when exposed to mould or other environmental toxins, as the liver Glucoronidation pathway is one of the primary detox pathways for mould toxins.
We all have Bilirubin in our blood, and its levels fluctuate and usually sit (for most people) below 15umoL.
In people with Gilbert’s Syndrome, there are chronic elevations of Bilirubin>17 umoL, often over 25 or 30 umoL, such as in the example below:
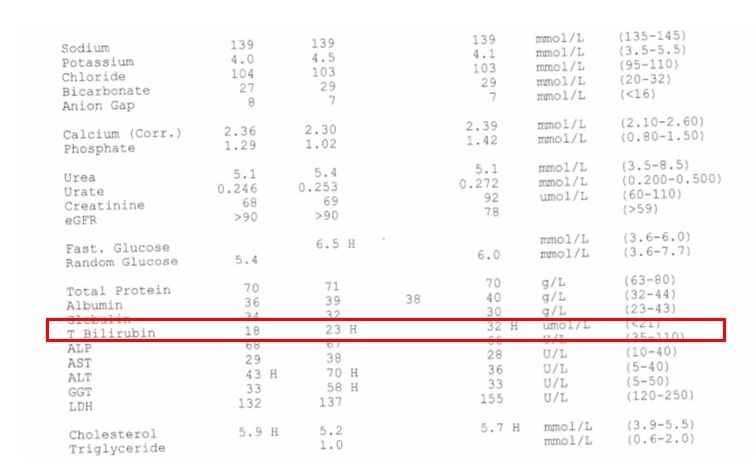
Continuously elevated bilirubin on Biochemistry blood test
Continuously high Bilirubin on Biochemistry blood test
The Syndrome was first described in 1901, affecting about 10-15% of Caucasians. With the higher incidence in Middle Eastern heritage (up to 25% of the population) and South-East Asians.
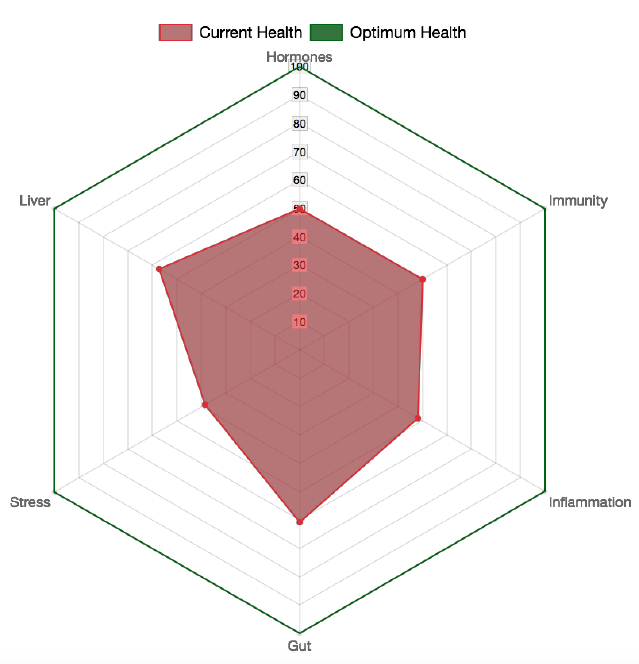
Summary of effects on the body from Gilbert’s Syndrome
- Predisposition to gallstones and gallbladder issues (more on this below).
- Slower intestinal motility and predisposition to SIBO(more on this below) and bowel flora imbalances, IBS and leaky gut. Often this is expressed via symptoms like nausea, food intolerances, bloating and ‘that heavy feeling in the stomach as if food sits there like a brick for hours’, and poor hunger in the morning.
- Anxiety and depression as well as mood fluctuations, panic attacks.
- Significantly reduced handling of paracetamol, aspirin and non-steroidal anti-inflammatories (NSAIDs) toxicity- the effects of these drugs on the liver of those with Gilbert’s is much greater than an average person and people with Gilbert’s need to exercise more caution with doses of these medications.
- Impaired handling of dopamine (our motivation and reward neurotransmitter) and estrogen. Clinically I find that when there are COMT and PEMT snps present combined with Gilbert’s, there is usually an issue with mood, anxiety, and depression. As well as definite estrogen dominance symptoms such as migraines, headaches, menstrual issues such as heavy bleeding/clotting and conditions such as endometriosis and fibroids as well as fibrocystic breasts and breast cancer.
- Poor stress tolerance, especially in a fasted state. People with Gilbert’s should avoid long periods of fasting,during which more Bilirubin is released.
The absolute key issue to address for anyone with Gilbert’s is gut health. If you are experiencing ongoing gut issues such as:
- pain
- feeling bloated with irregular bowel movements
- diarrhoea
- loose stools
- constipation
- or alternate between all of them
- food reactions and many others
My ONLINE PROGRAM – HEALING IBS – is an excellent start.
The Healing IBS program will guide you through a 5-week elimination and re-introduction diet as well as provide worksheets and recordings to re-program your stress response and calm your nerves, which calms the gut.
Gilbert’s Syndrome – Gut Symptoms
The UGT enzymes are expressed throughout the gastrointestinal tract, so issues in Gilbert’s can present as varying gut problems.
In the liver, glucuronidation is a key process in phase 2 detox, used to detoxify environmental toxins, pesticides, drugs, and hormones such as estrogen and testosterone, absorb fat-soluble vitamins A, D, E and K and produce melatonin.
In Gilbert’s, the enzymes (such as UGT) involved in this process are working far from optimally.
One of the functions of this liver pathway is to escort Bilirubin out of the body as it is a toxic by-product of metabolism. The liver conjugates (binds) Bilirubin by binding it to glucuronides. This function doesn’t work well in Gilbert’s Syndrome. Bilirubin ends up being only partially conjugated when mixing with bile, and this step is easily undone. It ends up being only partly conjugated.
Beta-glucuronidase is an important enzyme in the gallbladder, and large intestine that helps with this function- this enzyme is made by some gut bacteria species endogenously.
When Bilirubin comes in contact with beta-glucuronidase, it becomes unconjugated again and keeps circulating. Unconjugated Bilirubin is not water-soluble, which means the liver is not able to excrete it, so it just gets reabsorbed by the body again and again.
When glucuronidation is not working as it should due to genetic glitches or other liver pathology (sometimes alcoholism or drug use), the unconjugated Bilirubin builds up in the blood with toxic effects.
High Bilirubin impacts intestinal health negatively because it changes the behaviour of the intestine. It causes re-distribution of the tight junctions of the intestine, setting up a leaky gut and leading to food intolerances and parasite/bacterial overload.
A leaky gut has major implications for the functioning of the gut as well as a predisposition to autoimmunity.
Problems often manifest in the stomach- significantly delayed gastric emptying is very common. Studies have shown that in Gilbert’s, food stays in the stomach for up to 3 hours, which is roughly double the amount of time compared to those who don’t have Gilbert’s.
This is why people with Gilbert’s Syndrome often complain about burping and general upper gastric discomfort. At the same time, there is a tendency to have faster transit time in the intestine.
SIBO and Dysbiosis
The slower transit time often predisposes Gilbert’s people to SIBO (Small Intestine Bacterial Overgrowth) – an overgrowth of good and bad bacteria in the small intestine, where they are not meant to be or where there are not meant to be this many of them.
SIBO triggers many symptoms such as food intolerances, severe bloating and abdominal pain, often constipation but sometimes diarrhoea, reflux and even skin rashes and joint pains.
A common sign of SIBO is poor sugar and carb tolerance, so when people eat simple carbs like potato/sweet potato or fruits such as apples, they will get fairly immediate bloating/cramping/discomfort.
Nutrient deficiencies are always present with SIBO and will usually mean low levels of iron, magnesium, zinc, calcium and vitamin B12 as well as poor absorption of protein – thereby low levels of mood-enhancing amino acids. SIBO can also contribute to a leaky gut as the bacteria damage the intestinal lining leading to all the issues described above.
“Intestinal bacterial overgrowth occurs in several pathologic conditions and may result in increased bile salt and bilirubin deconjugation in the small intestine” ( Vítek, L and C. Carey, M, “New pathophysiological concepts underlying pathogenesis of pigment gallstones”, Clin Res Hepatol Gastroenterol. 2012 April ; 36(2): 122–129)
In the colon, the microbiome can be greatly influenced in Gilbert’s, predisposing to the growth of unfavourable species, particularly Clostridia species and Bacteroides Fragilis that process excess Bilirubin.

What we do know is that undigested starch in high carbohydrate diets and a high intake of refined sugars affects the metabolism of intestinal microflora and prolongs intestinal transit time, leading to perfect conditions for gallstones to develop, especially for those with Gilbert’s. (Vítek, L and C. Carey, M, “New pathophysiological concepts underlying pathogenesis of pigment gallstones”, Clin Res Hepatol Gastroenterol. 2012 April; 36(2): 122–129)
Gallbladder and Gallstones
The gallbladder is the critical organ for Gilbert’s Syndrome – the main highway for bilirubin excretion. What happens in Gilbert’s is that partly detoxified Bilirubin gets re-toxified in the gallbladder. This can lead to the formation of gallstones.
Having constantly high Bilirubin is a definite risk factor for gallstones and gallbladder sludge.
A study that looked at bile composition found that “The proportion of total bilirubin that was unconjugated was significantly higher in the bile from patients with stones than in bile from control patients” (Dutt M.K et al, “Unconjugated bilirubin in human bile: the nucleating factor in cholesterol cholelithiasis?’, J Clin Pathol 2003;56:596–598).
People with Gilbert’s have a higher rate of gallbladder issues such as gallbladder sludge, higher rates of ‘black stones’ (the most common gallstone that affects both children and adults). Increased Bilirubin reduces gallbladder motility, leading to this sludge formation:
“Increased proportions of unconjugated bilirubin in gallbladder bile may be a consequence of impaired gallbladder motility” and “Unconjugated bilirubin has been identified as a component of biliary sludge, which is believed to precede gallstones, particularly pigmented stones” (Dutt M.K et al, “Unconjugated bilirubin in human bile: the nucleating factor in cholesterol cholelithiasis?’, J Clin Pathol 2003;56:596–598).
Of course, not all Gilbert’s people have gallstones, but most will have symptoms of poor fat tolerance, such as nausea and poor ability to digest fatty foods and may feel pain in the diaphragm area.
Gilbert’s disease and the brain
Impaired bilirubin detoxification leads to impaired dopamine handling due to issues in the phase 2 pathway of the liver.
Impaired bilirubin detoxification leads to an increase in glutamate in the brain- glutamate is toxic to the neurons and damages the cell lining in the brain. Disturbing mood and sleep are often present during high levels of Bilirubin in Gilbert’s.
Also, because bilirubin build-up leads to increased intestinal permeability (leaky gut), the blood-brain barrier function in those with Gilbert’s will likely be altered, allowing for gut toxicity to impact the brain. This toxicity (from LPS- bacterial lipopolysaccharides) often leads to inflammatory conditions such as depression. Inflammation leads to nervous system stress and will always present with mood/brain issues.
This is an example of the gut-brain axis at work. Fascinating how everything is connected, isn’t it!
Usually, people experience diverse digestive symptoms that change from day to day and month to month, and often these have not been diagnosed by conventional medicine. The gastrointestinal tract is the way Bilirubin gets detoxified.
Clinically many of my clients suffering from long-term depression or anxiety often show up positive for Pyrroles and Gilbert’s Syndrome.
Fasting is completely contra-indicated for Gilbert’s Disease
No matter how often I have tried fasting or similar food restriction strategies over the last 20 years of dietary experimentation. I have never been able to do it well without significant detrimental effects like worsening gut issues, terrible mood and other ‘detox’ effects.
In truth, these are not detox effects but a massive spike in bilirubin levels produced by slowed gut function during fasting.
If you know you have high bilirubin levels. Even if you haven’t yet been diagnosed with Gilbert’s, you need to avoid long periods of fasting at all costs, as this will exacerbate gut and mental health issues over time.
What do I do if I have Gilbert Syndrome symptoms?
The first and most obvious is to look through your standard GP medical bloods under ‘Chemistry’ or ‘Biochemistry’ and read the Bilirubin line.
If it’s>15, you may have a problem. If you’ve had several historical readings >15 for many years, the chance you have Gilbert’s is very high.
Steps to take:
- Diagnosis: track bilirubin levels and do the genetic testing
- Education – things that increase Bilirubin include stress, fasting, synthetic estrogens, paracetamol, NSAIDs, recreational drugs that lead to high dopamine levels
- Take zinc! Zinc helps with anxiety, reduces glutamate, and binds unconjugated Bilirubin in the blood. To determine the correct form and dosage of zinc, see your trusted complementary health practitioner
- Support glucuronidation: several supplements can assist with liver detox function, Calcium d glucarate is one of them. Again, speak to your practitioner to ensure this is right for you.
- Support all phase 2 liver enzymes, particularly methylation, glutathionylation and sulfation, to reduce estrogen dominance. Cruciferous vegetables are great as they induce both glucuronidation and glutathionylation. For specific supplement support, speak to your practitioner. I also find liver function testing with each liver phase useful here.
- A lot of gut work throughout the stomach, liver, gut lining, and bowel to optimise digestion
- Antioxidants to reduce oxidative stress
Gilberts disease keys to treatment:
The goal is to get the unconjugated bilirubin levels into the ideal range and keep it there- this is a lifetime strategy due to the genetic nature of this condition.
- Reduce transit time and gastric emptying – speed up the rate at which food moves through the digestive tract. This will reduce the re-toxification of Bilirubin.
- Increase bile flow- reduces stagnation of bile in the gallbladder
- Improve fat absorption or correct malabsorption issues
- Acidify the colon- reduces beta-glucuronidase species (such as E-coli and clostridia).
- Improve positive microbiota- bacteria that reduce Bilirubin
- Improve gap junctions/ reduce leaky gut
- For inflammatory conditions such as IBD, colitis, and Crohn’s- more Bilirubin will be made to reduce haem (which protects the gut lining). When inflammation is present, it must be addressed as it is feeding into the bilirubin overload
- Support liver glucuronidation pathways
Addressing Gilbert’s in myself and my clients constantly has meant that this is a key area of research and practice for me.
Here’s how True Foods Nutrition can help with Gilbert’s Syndrome
- My new ONLINE COURSE for Gilbert’s Syndrome is here! The most complete resource on Gilbert’s Syndrome: Living with Gilbert’s Syndrome – True Health Synergy (simplero.com)
- Listen to my detailed podcast on Gilbert’s Syndrome with FX Medicine.
- You can also follow my Instagram page Gilberts_Syndrome_Support for all things Gilbert’s, my clinical insights and recommendations.
- Learn how to manage your Gilbert’s symptoms long term.
- Book in a consult with Clinical Nutritionist Maria Allerton.
- Start addressing your gut and mental health today via a self-guided online program formulated based on my clinic protocols.
Acknowledgements: thank you to one of my mentors, Rachel Arthur ND for the research and clinical insights into Gilbert’s Syndrome which I have used in compiling this information.







I watched your video to get genetic testing for Gilbert’s. The website for MTHFRsupport.com doesn’t seem valid- it says it’s unavailable- is there another company you recommend to forward the raw data to?
Thanks
Hi Tammy, it’s now called mthfrsupport.org
A have GS 59 and have been searching 40 hrs for answers…you’ve answered so many just on this page. I can’t wait to take the course. QUESTION: is there a connection between the heavy metals & mold in my labs? Thanks, Patrick
Glad you found the info useful. Yes, mould and metals both add a huge toxic load.
Hi, I am 31 years old. I have an elevated Bilirubin around 32 with 2 measurements this year and in 2020. My Doc doesn’t see a reason to do the genetic test. what would be the possible different outcome if the genetic test were positive or negative?
Kind regards,
Max
Hi Max, there could be other reasons for elevated bilirubin so it’s always best to confirm with genetic test. If your doctor won’t do it, you can do it yourself, all the instructions are in my video here: https://youtu.be/9RHR73NNRzM?si=TB9nzNl5ssDLLPu5
So I have been diagnosed with Gilbert’s about 3 months ago. I’m 47 years old and I’ve never noticed any jaundice but I’ve always felt like something is going on in my belly. Why aren’t any of the symptoms you described found in medical literature?
Hi Erik, unfortunately mainstream medicine is not interested in addressing conditions that don’t have a drug prescription attached to them:), I recommend my comprehensive online course Living with Gilbert’s to help you learn all about the syndrome and strategies to address your symptoms: https://www.truefoodsnutrition.com.au/living-gilberts-syndrome-online-course/
If I’m already taking a multivitamin would adding a daily zinc supplement be too much zinc?
It needs to be tested with blood and hair mineral testing, everyone’s levels are completely individual
My son is 17 and has had high bilirubin his entire life. Recently, however, he began experiencing symptoms. It started out as stomache pain, fatigue, and headaches. We saw a Dr who did x-rays and a CBC and everything was fine. Two weeks later, he was still feeling bad. Second opinion said he was constipated. He began to experience body aches, hair loss, and confusion. Third visit said GS. However, I am not so sure that it is it. All my research and even the doctors said GS is mild. My son is losing weight and hair and I am so concerned. We are going for another appointment in a couple of weeks. I am going to have his thyroid tested and CRP, ANA. My kid should be out with his friends, not frailing away.
Hi Shona,
Sorry to hear about your son. If you would like help to get to the root causes of his issues please book in with Eliza Blackwood on my team.
I have GS but I’m more concerned about my 20 year old daughter. Of course she inherited the “bad” genes from me but her dad does not have GS. I have found conflicting information on whether or not being heterozygous for the UGT1A1 genes can cause problems. She’s got the whole list of GS symptoms (horrible periods, anxiety, panic attacks, bowel issues, sleep issues, intolerance of hormonal birth control, etc). Before I invest in the course, is it possible to be heterozygous and affected? Or should I be looking at other things to help her?
Hi Nancy, yes I have several clients who are heterozygous and still have symptoms. The genes can still express depending on toxic load, environment, stress and many other factors. I recommend the course to anyone who is having the symptoms regardless of the genes. Hope that helps.
I’m really struggling, been told I have gastroparesis. My bilirubin is over 20. I have Gilbert’s. I believe that Keto/carnivore can help with my insulin resistance and highish blood pressure, but also it can be bad for Gilbert’s,especially the higher fat content. Please advise. I also had a large fibroid and hysterectomy 14 years ago. Yes possibly oestrogen dominance. Not sure what to do for the best. 🙏
Hi Angela, I recommend my online course on GS to help answer all your questions: https://www.truefoodsnutrition.com.au/living-gilberts-syndrome-online-course/
I am also a medical student having the same condition , all i saw in this article was so satisfying and detailed i am so pleased to study it, now i want to know more about the history and exam findings of the pain like the onset frequency duration character progression aggreviating relieving factors association and management etc so if u plz guide us about pain
Hi there. It seems that not only do I have Gilbert’s syndrome, but also poor methylation. What specific liver function tests can I ask my functional doctor about in order to test each phase of liver detox? Thanks!
Hi Graden
Yes methylation issues are common in GS people. I discuss all the testing, nutrition and supplements in detail in my online course Living with GS:https://www.truefoodsnutrition.com.au/living-gilberts-syndrome-online-course/
thx
I have had high bilirubin on most of my blood tests and was told I have Gilbert’s syndrome. I’d like to confirm with DNA and also have family members check theirs. We have all done 23and me so I have the raw data but just not fully sure how to review the snps for Gilbert’s? Do you have direction/advice on that?
Thank you!
Hi Tiffany, here is a video I made on this topic that will explain how to check your UGT genes:
https://youtu.be/9RHR73NNRzM?si=jUXmph-ffmPcFv_o
Cheers
SO happy to come across your work. I was born with jaundice, high bilirubin starting in puberty, and later in life developed gallstones that caused chronic pancreatitis which then led to an aneurism in one of the arteries leading to my Pancreas. I really have suffered the trifecta here and am trying now at 56 years old to manage this so no further damage can be done. Doctors always dismiss the Gilbert’s Syndrome as “nothing to worry about”. I do not drink much because it makes me so ill but doctors always seem suspect be cause of my high liver enzyme readings. Where do I start with additional testing or supplements to help alleviate symptoms?
Hi Kelly,
Thanks for getting in touch. I recommend you start with my online course Living with Gilbert’s syndrome: https://www.truefoodsnutrition.com.au/living-gilberts-syndrome-online-course/
Reach out if you need one on one help, thx
Good Day.
I have GS but have been told it’s not a problem for years. I have really struggled over the years with moods, anxiety, on edge feeling, low moods and not able to function normally life is a big struggle for me a lot of days.
I now believe it is all related to my GS and the Dr is wrong but I don’t know where to start to help myself as my Dr won’t hear anything about it.
I asked for more testing, but was told no as it wouldn’t achieve anything anyway and was a waist.
Could you please help me with where to start?
I eat very healthily, and take supplements my naturopath recommended.
Hi Tammy, I recommend my online course Living with Gilbert’s Syndrome, it will explain everything about the condition and give you simple diet, lifestyle and supplement strategies to manage it and reduce/eliminate symptoms:
https://www.truefoodsnutrition.com.au/product/living-with-gilberts-syndrome-online-course/
Thank you.