How To Fix Irritable Bowel Syndrome (IBS) By Treating The Root Causes
IBS is not a disease in and of itself. It is a collection of symptoms caused by other health factors. Other factors are often overlooked or not looked into at all. They often leave you with symptom relief but no solutions to address the cause of the digestive distress!
But there is no need to live with the throws of IBS long-term. You can address Irritable Bowel Syndrome by testing your gut health to discover what’s causing the IBS symptoms. And then, you can make a clear plan to fix the cause and heal your gut.
Irritable Bowel Syndrome… Don’t you just love the diagnoses of exclusion and the term ‘syndrome’?!
For millions of people who experience digestive distress daily – and I was one of these people at 17 years old – the story goes something like this:
- you have bloating when eating some meals (can be after the same foods or completely random);
- constipation or difficulty going to the toilet or loose stools or diarrhoea or (even more fun) both alternating;
- you get bad gas and pain in the general gut area when you are stressed (seemingly regardless of what you eat);
- emotionally you feel like you have zero control over your body, and your gut is controlling you.
You get OCD about where the bathrooms are anywhere you go. And over time, start limiting social occasions to avoid feeling like you are spending half the time on the toilet and the embarrassment that goes with that.
When you see your doctor, the best-case scenario is:
- you get a test for coeliac disease (negative 99% of the time)
- possibly a test for lactose intolerance
- if you are sick enough, a colonoscopy/endoscopy to rule out Crohn’s or bowel cancer.
- You may even be told to see a dietitian and try a low Fodmap diet.
If all your tests are normal, you are told you have Irritable Bowel Syndrome – not a disease, a syndrome!
A syndrome is a collection of symptoms that don’t match any defined ‘disease’.
To say that this is a frustrating diagnosis for many is an understatement (who thought of ‘Irritable’ in the first place?? The bowel is not Irritable. It’s not in a mood!).
Worst case scenario – you get prescriptions for laxatives and anti-depressants and get told ‘this is all in your head’ and you need to ‘just relax ‘.
Been there, done that.
I knew nothing when I was diagnosed with IBS at 20 years old (after about 3 years of intermittent digestive symptoms, which started when I was doing my high school exams). There was zero advice given (actually, I think the doctor did say peppermint tea helps!).
It took me years of dietary trial and error to determine what foods and situations would set off my symptoms. Then I completed my nutrition qualification, and the rest is history.
In this blog, I will share with you:
Why I believe there is no such thing as IBS
And why I know there is ALWAYS a cause (or several) of your digestive symptoms and why it’s essential to uncover the causes to avoid misery for life.
First of all, do NOT accept the vague diagnosis of ‘Irritable Bowel Syndrome!’
There is always a cause for IBS. It just needs to be uncovered with proper gut testing.
When I conduct a GI Map Gut Test with my clients, 99% of the time, the reasons (there are usually multiple) for their IBS are blatantly clear.
And yes, sometimes a follow-up endoscopy/colonoscopy is required if the issue has progressed enough to warrant further investigation.
Below I will discuss the most common reasons behind and what is an IBS cure and Irritable Bowel Syndrome symptoms. However, your first starting point should be a comprehensive gut test like GI Map.
Common causes for Irritable Bowel Syndrome:
Gastro Episode
An episode of gastro (at any time in your life) is triggered by pathogenic bacteria that actually change how your gut operates. It doesn’t even need to be severe or ‘eventful’ gastro. The gastro bug may be long gone, but the fallout from that damage remains. How often have I heard my clients say, ‘Nothing has been the same since that trip to X place and the gastro I had there’.
The pioneering work of gastroenterologist and researcher Mark Pimentel, MD, indicates that IBS – at least in the case of some patients – may be an autoimmune disease triggered by food poisoning that damages the nerves of the small intestine.
Dr Pimentel has identified antibodies that are produced in the body in response to common bacterial infections such as Campylobacter jejuni, E. coli, Shigella, and Salmonella. When there is a case of severe food poisoning, the antibodies cross-react with a protein in our gut nerve cells called Vinculin.
This cross-reactive attack triggers an immune response that culminates in producing anti-vinculin antibodies. This leads to the destruction of the intestinal lining and tight junctions. This tight junction attack produces intestinal permeability (leaky gut) and changes the movement in the gut (dysmotility).
Faulty intestinal motility facilitates small intestinal bacterial overgrowth (SIBO) and triggers IBS symptoms.
Dr Pimentel’s research shows that this process is prevalent in people with IBS-D (diarrhoea dominant) and IBS-M (mixed).
However, the antibodies do not appear to be significantly elevated in people with IBS-C (constipation-predominant IBS) and, therefore, cannot be used to diagnose that particular form of IBS.
How can we address antibodies in people with IBS?
Until the antibody test is widely available, we can use the GI Map Test to identify pathogenic bacteria infections and begin treatment as well as gut repair and autoimmune diet protocols.
Food Intolerances
Common food intolerances such as gluten, dairy, soy, and corn (and most grains) become a problem and can trigger all types of Irritable Bowel Syndrome – ranging from constipation to diarrhoea.
To distinguish between different types of food reactions, read my previous blog – Understanding Food Intolerances.
The real reason foods become a problem is the loss of our immune tolerance, our Secretory IgA layer.
Production of sIgA is important to the normal function of the gastrointestinal mucosa as an immune barrier. It represents the first-line immune defence of the gastrointestinal tract. Elevated levels are associated with an unregulated immune response.
On the other hand, low sIgA levels are the most common picture I see in the clinic, with the GI Map tests demonstrating a very low defence system. A system that has been ‘worn out’ by reacting to food triggers, so low sIgA leads to increased sensitivity to foods. Several studies link stress and emotionality with levels of sIgA.
We know that stress is a major factor in IBS, so people experiencing higher than normal amounts of stress will have a weaker Secretory IgA defence system. These people have a much higher sensitivity to common foods, triggering painful IBS symptoms.
How can we address Secretory IgA in IBS sufferers?
Secretory IgA is one of the key markers we can measure on the GI Map test, and there are many strategies to improve this immune layer to reduce food intolerance reactions.

Inflammation
Inflammation can come from the wrong foods (eg: casein from dairy is extremely inflammatory for many people) and parasites and pathogenic bacteria.
How can we address inflammation in Irritable Bowel Syndrome?
Calprotectin is a well-established inflammation marker and can be measured on the GI Map gut test. If there is inflammation in the bowel, it’s important to eliminate as many sources of it as possible, usually involving a strict diet.
Bacterial Imbalance (or dysbiosis)
An overgrowth of opportunistic or pathogenic bacteria.
Usually, the most common reason for this is the overuse of antibiotics (at any time in your life, especially in childhood) that decimates the rich rainforest of beneficial bacteria in your gut.
These imbalances can be corrected once identified with the GI Map test and carefully addressed by a qualified and experienced health practitioner.
The reason why the Fodmap diet helps alleviate IBS symptoms is that overgrown bacteria in the small intestine and bowel feed on the easily fermentable gases from these foods. Which then triggers discomfort and pain.
Note that I said – alleviate symptoms. That is all the Fodmap diet does: reduce symptoms. Unlike commonly stated in the media, it is NOT how we treat IBS or cure Irritable Bowel Syndrome. Removing these food groups simply reduces the pain, gas, and sensitivity symptoms and yes, makes life more manageable.
I used to follow a strict Fodmap diet for my IBS for years because I didn’t know the root causes of my Irritable Bowel Syndrome.
Without identifying the root causes and treating them, people are left to be ‘Fodmap for life’, which is a very damaging approach in the long term.
Many Fodmap foods are actually highly beneficial as prebiotic fibre to our gut flora. Eliminating these foods eventually leads to worse dysbiosis!
This is an essential concept to understand if you are an IBS sufferer – the Fodmap diet is NOT a cure or treatment. It is a symptom relief approach that works well in the short term for some people.
How can we cure or fix IBS?
The key approach to fixing Irritable Bowel Syndrome is to do the full testing to identify YOUR root causes. Then address these so that you don’t have to eliminate healthy foods from your diet for the rest of your life. Working with a skilled practitioner is the best way to do this.
Bacterial overgrowth Sydney Nutritionist

Bacterial overgrowth Sydney Nutritionist
Parasites
Parasites are prevalent and responsible for many digestive symptoms.
Many people carry parasites. However, only some become symptomatic. The gut environment varies tremendously from person to person and is what determines whether parasite infections will lead to symptoms.
All parasites, however, drain our nutrient stores, so this is a vital area to address.
Dientoemeba Fragilis and Blastocystis Hominis are Australia’s two most common parasites. Regarding parasites, there are two schools of thought among traditional medical professionals such as GPs and gastroenterologists and complementary therapists such as nutritionists and naturopaths.
One school’s view is: to kill them. Kill them all and use the biggest guns we have – antibiotics (medical) or strong herbal antimicrobials (complimentary).
The second school’s view (which I tend to lean towards, depending on my client’s case) is: the parasite is not the problem. The terrain is the problem. In other words, the gut environment, the nutrient levels, the health conditions, and the stress/emotional health are the key drivers of allowing the parasite to take hold and cause trouble.
This ‘terrain’ – meaning our whole gut environment and digestion – starting from the mouth and ending in the anus is what requires work, and attempting to kill off a parasite may make the situation worse.
How can we address IBS?
The GI Map gut test tests for several common parasites and provides their quantities to measure treatment success.
Undiagnosed Helicobacter Pylori infection
Until I started using the GI Map Stool Test, I assumed that if a client came in with a negative H.Pylori breath test from their doctor, that ruled out this stomach infection. This is far from reality, it turns out.
Quite often, the breath test will provide a false negative if the bacterial levels are relatively low or if the bacteria are inactive at the time of the test.
H.Pylori can be a big trigger for IBS as it changes the stomach acidity and thereby predisposes the person to bacterial overgrowth in the small intestine (SIBO), a widespread cause of IBS. If you’d like to read more on low hydrochloric acid and SIBO, you can do so via this blog post, Gut Tests – What You Need to Know to Heal Your Gut.
How can we address H. Pylori?
The GI Map test identifies the DNA of H.Pylori and its virulence factors which is a far more accurate approach than just breath testing alone.
Identifying and treating H.Pylori infections naturally can significantly affect how you absorb nutrients and how your gut motility functions.
Poor stress management, past trauma, exhausted adrenals
Stress destroys our Secretory IgA immune layer, leaving us open to food sensitivity reactions.
Stress changes the hydrochloric acid, thereby altering the motility of the gut.
Stress reduces nutrient absorption, making everything more difficult.
In short, managing stress is a hugely important part of IBS resolution.

How can we address stress levels to help IBS?
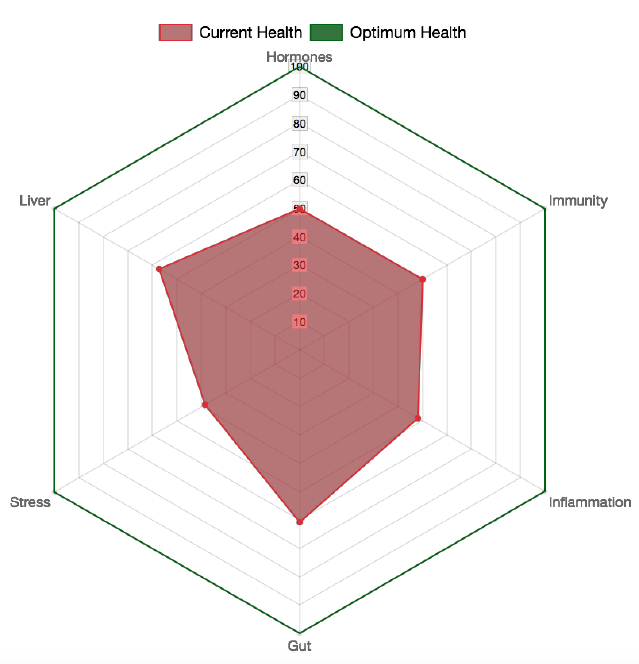
To address stress levels in the clinic, my clients undergo a Hair Tissue Mineral Analysis, which identifies adrenal and thyroid under function. Also, sometimes it’s essential to test the cortisol levels, done with a simple saliva test.
Once we have identified how stress affects your life, lifestyle strategies and targeted supplements can be used to reduce its impact.
Gut-directed hypnotherapy is one of the most effective and scientifically proven methods to manage stress and resolve Irritable Bowel Syndrome.
Hypnotherapy is used in our clinic both locally and via Skype successfully to drastically reduce stress levels and facilitate gut healing.
We will soon launch a unique online IBS Healing program that will address nutrition AND stress. This program will give you a step-by-step guide on managing your digestive symptoms and a roadmap to resolve them for good. Contact me for more information.
Want to know more about GI Map Gut Testing?
You can read more out GI Map Gut Testing or book an IBS consultation to discuss how your specific Irritable Bowel Syndrome needs can be addressed.
Ready to take action and finally fix your Irritable Bowel Syndrome?
Start today with my online HEALING IBS PROGRAM that guides you through:
- 5 week elimination and re-introduction diet
- 10 modules of stress reduction, mindfulness and hypnotherapy
It’s the simplest way to start addressing your IBS for good.









Hi there, can you please be my doctor lol:( do you take consultations or appointments and are in Australia? I need to see someone regarding my digestive issues I’ve had for the last 6 months and I really want someone with your mindset towards this issue because so often I get fobbed off by doctors:( I’m losing my mind
Lol yes I do, I consult via zoom anywhere in the world and am based in Sydney. You can book in with me or my team on the bookings page, thx
[…] are responsible for vague symptoms like headaches, behaviour changes such as anxiety/depression, digestive symptoms like IBS (irritable bowel syndrome), aches and pains (including arthritis type symptoms), reflux and indigestion, inability to lose […]