Could Fructose Be Your Trigger in Gilbert’s Syndrome?
Understanding fructose sensitivity and its link to liver health, energy production and Gilbert’s Syndrome.
Do you ever feel bloated, foggy, or fatigued after eating fruit, honey, or sweetened foods or especially after soft drinks or processed/fast foods? If so, fructose — a naturally occurring sugar in many fruits and sweeteners — might be a hidden culprit. This is especially relevant if you have a sensitive liver or conditions like Gilbert’s syndrome, which may amplify your response to certain sugars.
If you have Gilbert’s Syndrome and often experience fatigue and/or hypoglycemia (like I did for decades!), fructose could be a real problem.
Let’s unpack how fructose sensitivity affects the body, which foods are most problematic, and how you can test for fructose-related issues.
What is fructose, and why can it be a problem?
Fructose is a naturally occurring sugar found in various foods, particularly fruits and sweeteners, and is often discussed in relation to sensitivity to fructose.
Fructose can be found in:
- Fruit, fruit juices
- Honey, maple syrup and agave syrup
- High-fructose corn syrup -found in high quantities in energy drinks, processed foods and most fast foods
- Table sugar (sucrose is 50% fructose) and coconut sugar
- Sweetened beverages
- Xylitol and Sorbitol- both of which are converted into fructose in the body
While it’s “natural,” fructose is metabolised differently than glucose, placing a unique load on the liver.
How fructose affects your liver (and drains your energy)
Unlike glucose, fructose is almost entirely processed in the liver, in a similar way to alcohol! In the liver it:
- Uses up ATP (your cells’ energy currency) quickly
- Bypasses the usual regulatory steps in sugar metabolism
- Converts into fructose-1-phosphate, which:
- Depletes ATP
- Increases uric acid
- May contribute to oxidative stress and fatigue
Over time, this can cause:
- Low energy
- Poor stress tolerance
- Brain fog
- Raised bilirubin (animal studies)
- Worsened liver function in vulnerable individuals, like those with Gilbert’s syndrome
Fructose is metabolised primarily in the liver, where it must be processed by the enzymes fructokinase and aldolase B. While this metabolism is separate from bilirubin metabolism, some individuals with Gilbert’s report symptoms like fatigue, bloating, or brain fog after consuming fructose-rich foods.
Gilbert’s Syndrome: Why fructose may hit you harder
Fructose consumption increases bilirubin
A mouse study where the animals were fed a high fructose diet (were given a 30% fructose solution with their standard diet for 20 weeks) showed a significant increase in total bilirubin compared to the control group. All liver enzymes, inflammatory markers and blood triglycerides were also ALL markedly increased. The study then used quercetin to bring the numbers back in range, but not enough to fully reduce the damage from fructose. (“Regulatory Roles of Quercetin in Alleviating Fructose-Induced Hepatic Steatosis: Targeting Gut Microbiota and Inflammatory Metabolites”)
“Fructose overconsumption may result in insulin resistance, oxidative stress, inflammation, elevated uric acid levels, increased blood pressure, and increased triglyceride concentrations in both the blood and liver” (“Fructose and the liver”)
“Fructose is recognised as a major mediator of NAFLD (non alcoholic fatty liver disease), as a significant correlation between fructose intake and the degree of inflammation and fibrosis has been found in preclinical and clinical studies” (“Fructose and the liver”)
“During fructose metabolism, ATP depletion occurs and induces oxidative stress and inflammatory response, disturbing functions of local tissues and organs to overproduce inflammatory cytokines, adiponectin, leptin and endotoxin, which act as indirect dangerous factors. Fructose and its metabolites directly and/or indirectly cause oxidative stress, chronic inflammation, endothelial dysfunction, autophagy and increased intestinal permeability, and then further aggravate the metabolic syndrome with tissue and organ dysfunctions (“High Dietary Fructose: Direct or Indirect Dangerous Factors Disturbing Tissue and Organ Functions”)
Because the liver already has a reduced capacity to detoxify bilirubin efficiently in Gilbert’s, additional metabolic demands (like high fructose intake) may worsen symptoms or trigger episodes of provoked fatigue and discomfort.
Fructose malabsorption is a separate but overlapping issue — some people with Gilbert’s may also have fructose malabsorption or SIBO (Small intestine bacterial overgrowth), which can lead to GI symptoms when consuming excess fructose.
Fructose depletes ATP, making it so much harder for the liver to manage bilirubin and other functions
Fructose metabolism in the liver can rapidly deplete ATP (adenosine triphosphate) — the cell’s main energy currency — especially when consumed in large amounts. This happens due to the unique way fructose is processed, which bypasses key regulatory steps in glycolysis. Then uric acid rises and increases oxidative stress in the liver — this contributes to fatigue or poor stress tolerance in people with Gilbert’s.
Here is a short video that explains how fructose drains ATP and raises uric acid.
Consequences of ATP depletion from fructose:
- Oxidative stress ((due to uric acid and ROS (reactive oxygen species) generation))
- Mitochondrial dysfunction
- Impaired detoxification and energy metabolism
- Increased fatigue and poor tolerance to high sugar intake
Excess fructose has also been linked to:
- Non-alcoholic fatty liver disease (NAFLD)
- Insulin resistance
- Obesity and visceral fat gain
- High triglycerides
- Type 2 diabetes
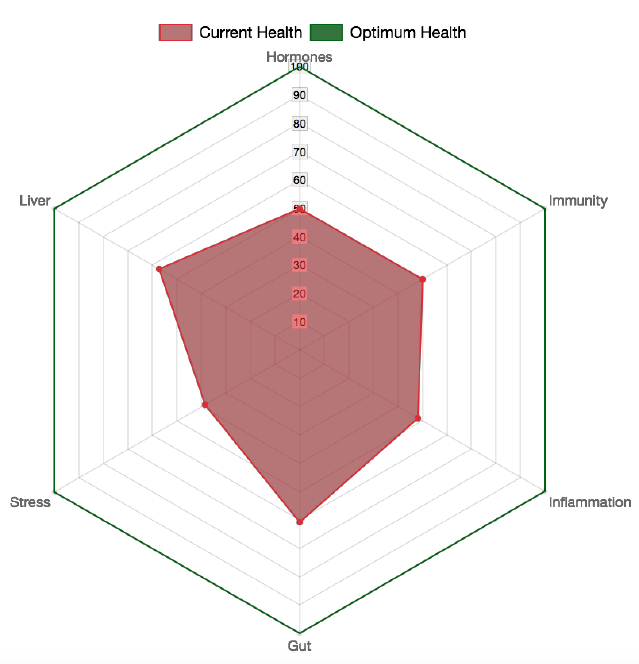
Why does this matter in conditions like Gilbert’s?
In people with Gilbert’s syndrome, the liver already has:
- Reduced UDP-glucuronosyltransferase (UGT1A1) activity
- A slightly compromised detox capacity
So, ATP depletion from fructose may further stress liver metabolism, worsen fatigue, detox symptoms, or bilirubin accumulation.
My recommendations for those with Gilbert’s
- People with Gilbert’s may feel better with a trial of limiting or avoiding high-fructose foods, especially:
- Sweetened beverages (fruit juice, soft drinks)
- Honey, agave, and high-fructose corn syrup
- Large amounts of fruit in one sitting
A low-fructose or moderate-fructose diet for 1-2 months may be worth trialing if you experience:
- Fatigue
- Brain fog
- Mood swings
- Hypoglycemia
- Sluggish digestion
- Have a history of IBS, SIBO, or food sensitivities
- Bloating or excessive gas, especially if any of the above are worse after eating high fructose foods (see list below). Try it for yourself for a period of at least a month and see if you feel better. This strategy is especially worthwhile if you already have fatty liver, gallbladder issues or any diagnosed liver symptoms and especially if you are overweight in the abdominal area.
High-fructose foods to limit or avoid
These foods are high in free fructose or have a high fructose-to-glucose ratio, making them harder to absorb and more likely to trigger symptoms, especially for people sensitive to fructose (e.g. with fructose malabsorption, IBS or Gilbert’s syndrome):
These contain more fructose than glucose, and often in high total amounts:
| Fruit | Fructose (per 100g) | Notes |
| Apples | ~6 g | Especially in juices or dried |
| Pears | ~6–7 g | One of the highest |
| Watermelon | ~3.4 g | High in fructose and FODMAPs |
| Mango | ~4.7 g | Also high in sorbitol |
| Cherries | ~5.4 g | Can be problematic in quantity |
| Grapes | ~7–8 g | Very high sugar overall |
| Honeydew melon | ~3.1 g | Moderate |
| Lychee | ~4.1 g | Watch portion size |
| Dried fruits (raisins, etc.) | ~15–30 g | Extremely concentrated sugars |
Sweeteners high in Fructose (Avoid)
- Honey
- Agave syrup
- Coconut sugar and syrup
- Maple syrup
- Xylitol (converts to fructose in the liver)
- Sorbitol (converts to fructose in the liver)
Sweeteners that don’t contain or don’t convert to Fructose (OK to have on low fructose diet)
- Stevia
- Monk fruit
- Erythriol
- Maltodextrin (not ideal but is often added to foods and supplements)

Foods highest in high-fructose corn syrup (HFCS):
- Soft drinks- all
- Sports drinks
- Fruit punches and fruit cocktails
- Iced teas
- Energy drinks
- Flavoured waters with added sweeteners
- Sweetened coffee drinks
- Processed sweets: candy, commercial chocolate, chewing gum, marshmallows, frostings/glazes
- Baked goods: packaged muffins and cupcakes, cake mixes
- Donuts and pastries, especially frosted
- Sweetened breads (eg: raisin bread)
- Sweetened cereals (most kids cereals), granola bars, breakfast bars, flavoured instant oatmeal, pudding cups and snack packs
- Condiments and sauces: ketchup, bbq sauce, salad dressings (especially honey mustard or ‘french’), teriyaki sauce, relishes and chutneys
- Dairy and frozen desserts: flavoured yogurts, ice cream and frozen yogurt, whipped toppings, milkshakes from fast food outlets
- Takeaway and fast foods: burger buns and sweet sauces, glazed or sweetened meats, chain restaurants salad dressings and dips
- Hidden HFCS sources to watch: ‘Natural’ fruit drinks, canned fruits in syrup, kids multivitamins or chewables, flavoured nut butters, sweetened nut milks and protein shakes, some cough syrups and lozenges
Which may all affect your liver health if consumed excessively.
When reading labels, look out for:
- High fructose corn syrup
- Corn syrup solids
- Glucose-fructose syrup
- Isoglucose
- Maize syrup
By recognising foods that have fructose and their effects on your body, including the need to monitor your intake of high fructose foods, you can better manage fructose sensitivity symptoms and improve your liver health.
My recommendation is to avoid ALL processed food and drinks that contain any form of high fructose corn syrup.
Moderate-fructose foods – better tolerated (watch portion size)
These may be tolerated in small amounts, especially when eaten with protein or fat
(Fructose ≤ Glucose — easier to absorb)
| Fruit | Fructose per 100g |
| Bananas | ~4.9 g |
| Strawberries | ~2.5 g |
| Citrus fruits | ~2–3 g |
| Blueberries | ~3.5 g |
| Kiwi | ~4 g |
| Raspberries | ~1.5 g |
| Avocado | Negligible |
Low-fructose and fructose-friendly foods
If you’re concerned about your sensitivity to fructose, consider incorporating fruits low in fructose.
These are generally better tolerated and can form the base of a low-fructose plan.
Low fructose fruits (safer options)
These fruits with the least fructose can be delicious alternatives that promote overall health without aggravating your symptoms:
- Berries (strawberries, blueberries, raspberries, blackberries)
- Citrus fruits (oranges, mandarins, lemon, lime, grapefruit)
- Avocado
- Unripe bananas
- Rhubarb
- Kiwi (for some)
Vegetables (all low-fructose):
- Leafy greens (spinach, kale, lettuce)
- Zucchini
- Pumpkin
- Carrots
- Cucumber
- Green beans
- Broccoli (in moderation)
- Eggplant
- Capsicum (in moderation)
Others:
- Protein (meat, eggs, fish)
- Fats (olive oil, nuts, seeds)
- Whole grains (quinoa, rice, oats)- only if tolerated
- Lactose-free dairy or plant-based alternatives (unsweetened)- eg, unsweetened almond milk
- Herbal teas and water
What tests can detect fructose sensitivity?
If you suspect fructose is contributing to your symptoms, testing can help clarify the picture.
1. Fructose Hydrogen Breath Test (part of SIBO testing)
- Drink a fructose solution, then measure breath hydrogen/methane.
- If your small intestine doesn’t absorb fructose properly, bacteria ferment it, → gas is released and measured.
- Used to diagnose: Fructose malabsorption
- True Foods Nutrition can order all SIBO testing
2. Genetic Test for Hereditary Fructose Intolerance (HFI)
- A rare genetic liver disorder diagnosed via ALDOB gene testing.
- Symptoms include nausea, vomiting, and liver problems in infants/children after eating fructose or sucrose.
- Not the same as fructose malabsorption — but important to rule out in patients with strong reactions.
3. Additional/Supportive Testing
These aren’t diagnostic but may point toward downstream effects of fructose overload:
- Uric acid levels (may be elevated with high fructose intake)
- Liver function tests (LFTs)
- Organic Acids Test to understand mitochondrial function
- SIBO breath test (Small Intestinal Bacterial Overgrowth can worsen fructose intolerance)
- Comprehensive stool test (gut flora imbalance may impair fructose absorption)
What you can do
- Try a low-fructose diet for 3–4 weeks to see if symptoms improve.
- Stick to better-tolerated fruits and avoid high-fructose sweeteners (e.g. agave, high-fructose corn syrup).
- Support liver function with gentle liver nutrients (like B vitamins, magnesium, and taurine).
- Work with a practitioner to rule out SIBO, malabsorption issues and mitochondrial dysfunction
Final thoughts on sensitivity to fructose
Fructose is not a poison, but it can be toxic at modern dietary levels, especially from added sugars in drinks and processed foods. Whole fruits in moderation are generally safe and beneficial for most people.
While fructose isn’t inherently “bad,” your body’s ability to handle it varies, especially if you have Gilbert’s Syndrome or other liver sensitivities. By understanding how fructose affects your system and taking the right steps to assess tolerance, you can reclaim your energy, reduce digestive discomfort, and better support your metabolic health.
For more on Gilbert’s Syndrome
- Read my detailed article: Gilbert’s Syndrome and High Bilirubin: Learn Hidden Cause of Gut/Brain Issues.
- Visit my super comprehensive ONLINE COURSE: Living with Gilbert’s Syndrome.
The online course contains a very detailed module on fructose and Gilbert’s, as well as ways to restore energy and ATP production after fructose issues. It also contains a detailed understanding of GS, food and supplement strategies and all the relevant info on blood and functional medicine tests.
Blog References:
- “Fructose and the Liver”, Pablo Muriel et al, Int J Mol Sci, 2021 Jun 28;22(13):6969, doi: 10.3390/ijms22136969.
- “Fructose overconsumption-induced reprogramming of microglia metabolism and function”, Kenneth K Y Ting, Front Immunol, 2024 Mar 26:15:1375453. doi: 0.3389/fimmu.2024.1375453.
- “High Dietary Fructose: Direct or Indirect Dangerous Factors Disturbing Tissue and Organ Functions” Dong-Mei Zhang et al, Nutrients, 2017 Mar 29;9(4):335. doi: 0.3390/nu9040335.
- “Regulatory Roles of Quercetin in Alleviating Fructose- Induced Hepatic Steatosis: Targeting Gut Microbiota and Inflammatory Metabolites”, JinjunLi et al, Food Sci Nutr, 2024 Dec 20;13(1):e4612. doi: 10.1002/fsn3.4612